Navigating Emotions: Understanding Postpartum Depression
The arrival of a new baby brings bundles of joy, giggles, and countless precious moments. However, for some new mothers, it also brings a range of emotions that might not align with the expected happiness. Postpartum depression, often referred to as PPD, is a real and challenging experience that impacts many new mothers. In this guide, we’ll explore postpartum depression in simple terms, helping to shed light on this common yet often misunderstood condition.
- Defining Postpartum Depression: Postpartum depression is a form of depression that occurs after giving birth. It’s different from the “baby blues,” which are common feelings of sadness or weepiness that many mothers experience in the first week or two after childbirth. Postpartum depression involves more intense and prolonged feelings of sadness, hopelessness, and anxiety that can interfere with a mother’s ability to care for herself and her baby.
- Common Symptoms: Understanding postpartum depression begins with recognizing its symptoms. These can include persistent feelings of sadness or emptiness, a lack of interest or pleasure in activities, changes in appetite and sleep patterns, excessive fatigue, feelings of guilt or worthlessness, difficulty concentrating, and thoughts of self-harm or harming the baby. It’s crucial to remember that symptoms can vary, and not every mother with postpartum depression experiences the same set of challenges.
- Onset and Duration: Postpartum depression can begin any time during the first year after giving birth, but it typically starts within the first few weeks to months. It’s essential to be aware of the duration and intensity of these feelings. If symptoms persist and interfere with daily functioning, seeking help is crucial.
- Risk Factors: Certain factors may increase the risk of developing postpartum depression. These include a history of depression or anxiety, a lack of a strong support system, stressful life events, complications during pregnancy or childbirth, and hormonal changes. While these factors may contribute, postpartum depression can affect any new mother.
- Hormonal Changes: Hormonal changes play a role in postpartum depression. The sudden drop in hormones, particularly estrogen and progesterone, after childbirth can contribute to mood swings and emotional challenges. Additionally, thyroid hormone levels may fluctuate, further impacting mood and energy levels.
- Importance of Seeking Help: Seeking help for postpartum depression is crucial for both the mother and the baby. It’s not a sign of weakness but a proactive step toward getting the support needed for emotional well-being. Many effective treatments and support systems are available to help mothers navigate through this challenging period.
- Talking About Feelings: One of the first steps in addressing postpartum depression is talking about feelings openly. It’s okay for mothers to share their emotions, concerns, and challenges with healthcare providers, partners, family, or friends. This can create a supportive environment and pave the way for seeking professional help.
- Healthcare Provider Guidance: Healthcare providers play a vital role in supporting mothers with postpartum depression. Regular check-ups during the postpartum period provide opportunities to discuss emotional well-being, and healthcare professionals can offer guidance on treatment options, including therapy, medication, or a combination of both.
- Therapeutic Approaches: Therapy, particularly talk therapy or counseling, is a common and effective approach for treating postpartum depression. Therapy provides a safe space for mothers to explore and express their feelings, learn coping strategies, and receive guidance on managing the challenges of motherhood.
- Medication Options: In some cases, medication may be recommended to manage the symptoms of postpartum depression. Antidepressant medications, when prescribed and monitored by a healthcare provider, can be a valuable part of a comprehensive treatment plan. It’s essential for mothers to discuss any concerns or questions about medications with their healthcare provider.
- Support Groups: Joining a postpartum depression support group can be a comforting and validating experience. Connecting with other mothers who are facing similar challenges provides a sense of community and reduces feelings of isolation. Many communities offer local or online support groups where mothers can share their experiences and offer mutual support.
- Partner and Family Support: The support of partners and family members is crucial for a mother navigating postpartum depression. Partners can play an active role in providing emotional support, helping with baby care responsibilities, and creating a nurturing environment. Open communication within the family is key to fostering understanding and empathy.
- Self-Care Practices: Incorporating self-care practices is an essential aspect of managing postpartum depression. This includes prioritizing rest, engaging in activities that bring joy, setting realistic expectations, and seeking moments of solitude. Mothers should not hesitate to ask for help and take breaks when needed.
- Balancing Responsibilities: Balancing responsibilities as a mother with postpartum depression involves finding a rhythm that works for both the mother and the baby. Partners and family members can assist with daily tasks, allowing the mother to focus on self-care and gradually reintroducing personal and work-related responsibilities.
- Gradual Return to Daily Activities: A gradual return to daily activities is a positive step in the postpartum depression journey. Setting small, achievable goals, such as going for a short walk or engaging in a hobby, helps build a sense of accomplishment and promotes a gradual return to routine.
- Managing Expectations: Managing expectations during postpartum depression is crucial. Accepting that each day may present different challenges and victories allows mothers to navigate the journey with greater flexibility and self-compassion. Celebrating small achievements contributes to a positive mindset.
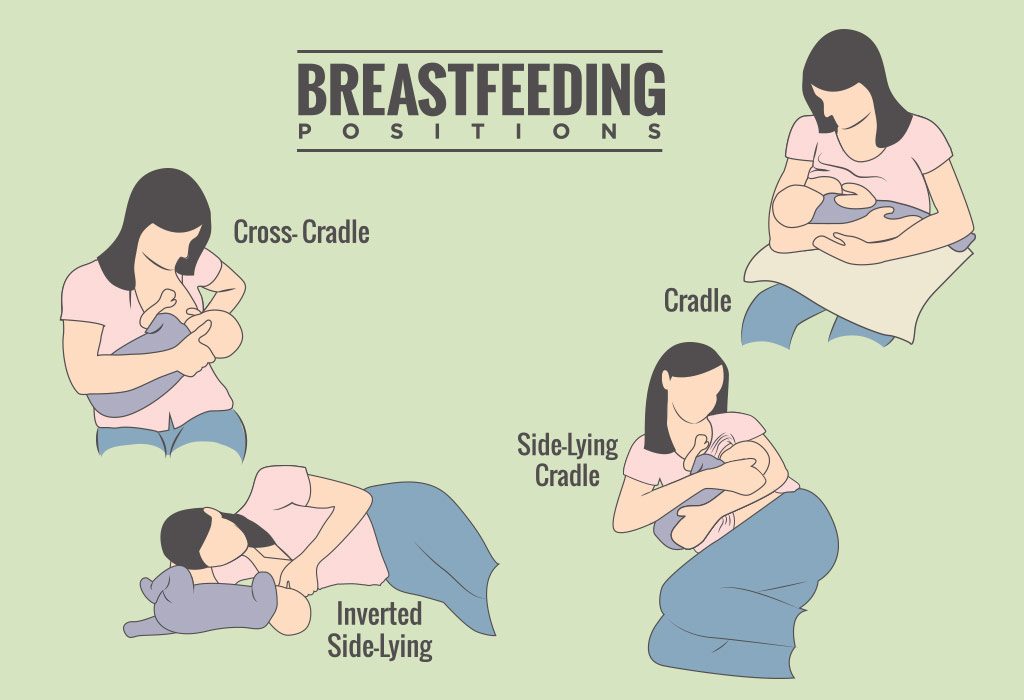
- Impact on Parent-Child Bond: Postpartum depression can impact the parent-child bond, but with support and treatment, this bond can be strengthened over time. Engaging in activities that promote bonding, such as skin-to-skin contact, gentle play, and shared moments of comfort, fosters a positive connection.
- Encouraging Open Communication: Encouraging open communication within the family is vital. Partners and family members can express their support and understanding, providing a safe space for the mother to share her feelings and concerns. A united front in addressing postpartum depression creates a supportive environment.
- Understanding Treatment Progress: Understanding that the road to recovery from postpartum depression is a gradual process is important. It’s common for mothers to experience ups and downs, and progress may take time. Celebrating small victories and acknowledging progress, no matter how gradual, contributes to a positive outlook.
- Celebrating Resilience: Finally, celebrating the resilience of mothers facing postpartum depression is essential. Acknowledging the strength it takes to seek help, engage in treatment, and navigate the challenges of motherhood demonstrates the power of resilience. Every step forward, no matter how small, is a testament to the courage and strength of mothers on this journey.
Conclusion:
Postpartum depression is a significant and often challenging aspect of the postpartum period. Understanding this condition in simple terms allows mothers, partners, and support networks to approach it with empathy, awareness, and a commitment to seeking help when needed. By fostering open communication, accessing professional support, and embracing self-care practices, mothers can navigate postpartum depression with resilience and gradually move towards a brighter, more emotionally balanced future.